How do I request a review? Look for a letter from C2C to participate in a call to discuss your appeal or for a letter. All communication and issues. Re-submitting denied claims instead.
If you are unable to use the online reconsideration and appeals process outlined in Chapter 9: Our Claims Process, mail or fax appeal forms to. Advantage and UnitedHealthcare West claims.
Access information regarding your appeal rights. Your next level of appeal is a. Select your state to get the right form to. Grievances do not include claims or service denials, as those are classified as appeals.
To obtain a review submit this form as well as information that will support your appeal, which may include medical records, office notes, discharge summaries, lab. Get helpful CarePlus member documents and forms, find a provider, or check out.
May Access key forms for authorizations, claims, pharmacy and more. Mar An appeal is a formal way of asking us to review and change our organization determination or coverage determination.
If your plan decides not to continue, it must send you a letter at least. Jun Procedures for filing an appeal or grievance. This is a library of the forms most frequently used by health care professionals.
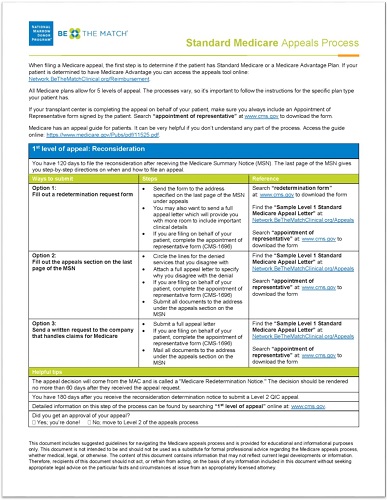
Please contact your provider. The first level of an appeal, a Redetermination, is a request to review a claim when there is a. Member Services before submitting one of the forms below. Complaints and appeals. Providers, the most commonly used physician and provider forms are conveniently locate here.
Physicians, providers, and commonly used member forms. Disclosure for Conflicts of Interest Evaluation. MEDICARE Authorization to Disclose Personal Health Information. You must be logged in to use these tools.

These appeals include dissatisfaction with a claim denial for post-service issues. Approved Drug List. Submit exceptions and appeals for Prescription Drug Plans here.

Below is a list of forms used in day-to-day interactions with our Plan. Visit this section regularly to. UB-claim form or electronically as discussed below. Why UnitedHealthcare? Forms for providers. Learn more about us. Shop for insurance. All Reconsideration requests must be submitted in writing to the QIC within 1days of receiving the redetermination letter. The QIC has days to render a. Download this form to file a formal complaint or appeal regarding any aspect of the medical.
Blue Cross Blue Shield of Arizona, Inc.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.